WMIF MAIN SITE
2025 Event Site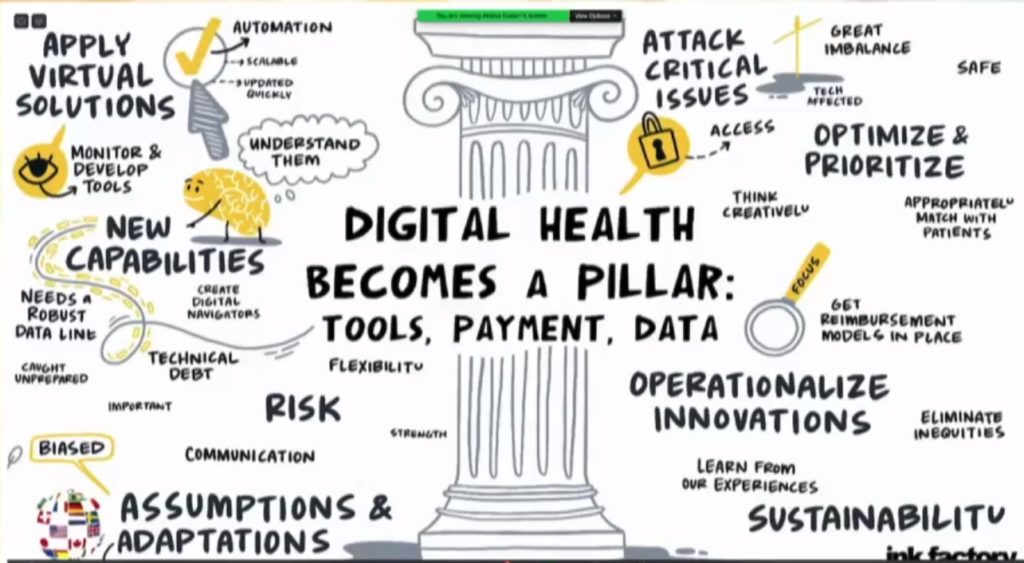
Deployed in the crucible of the coronavirus pandemic, digital health has now become an essential pillar in the delivery of care. Alistair Erskine, MD of Mass General Brigham, Adam Landman, MD of Brigham Health, Brooke LeVasseur of AristaMD, and Lee Schwamm, MD of Massachusetts General Hospital discuss how the outbreak of COVID-19 accelerated the use of digital health and the risks and adaptations that have followed.
Lee Schwamm, MD explained some of the virtual care workstreams that emerged: “We needed better ways to care for our patients inside their isolated hospital beds and rooms. We leveraged a video intercom solution so that patients could have a humane physical contact experience over the iPad with their providers while limiting the use of PPE and personal exposure.”
Further, technology was used for monitoring of patient trends and identifying opportunities for intervention early, before deterioration began. In order to keep people out of the hospital altogether, virtual urgent care ramped up to address minor concerns or manage other chronic conditions. Lastly, automation was further developed using health bots to assist in getting COVID information out, providing web-facing experiences for patients with questions, and assisting with employees’ occupational health needs during the crisis. All of this was designed to be scalable and to be updated on a moment’s notice.
There are several costs and challenges to sustaining this kind of work. Alistair Erskine, MD stated: “It is important that we understand what new critical capabilities we need to have. For example, to be able to adapt during uncertain times, making changes to digital health technologies on the fly, and being able to rapidly deploy search capabilities. We also added virtual as a standard venue in the care model. All of this requires a more robust and refined data environment.”
Brooke LeVasseur shared some insight on how she sees interactions in the near term between industry and clinical institutions: “As we look towards trying to operationalize a lot of these new innovations with partners, it is important that as an industry we recognize that there isn’t going to be a one size fits all solution, so we have to take into context the unique needs of each institution. They each have their own unique market, dynamics, and populations that they’re serving, and that all must be baked into a deployment and sustainability strategy. Lastly, without a lasting sustainable economic model, these innovations will not be able to continue. As an industry, we need to be focused on working to get reimbursement models in place that reflect the value that these innovation models can deliver.”
How do we begin to handle issues around clinical appropriateness, reimbursement, regulatory concerns, and equity? Adam Landman, MD discussed the sustainability of telehealth and its astronomical increase in use. “Some would say we’ve had years of work happen in a matter of weeks. My biggest concern is that we will lose this digital transformation in health due to reimbursement. Before COVID-19, there was really limited reimbursement for telehealth. Now, some states and some insurers have agreed to cover telehealth services at parity with inpatient. The big question is whether that will continue. It is my sincere hope that we can work with the federal and state policymakers and insurers to find the right balance to be able to offer telehealth services when appropriate and to find the most appropriate reimbursement to incentivize their use.”
There have been multiple assumptions about what digital health could do and multiple ways in which adaptations occurred over the past couple of months. “We had some assumptions that were prejudices or biases,” Schwamm explained. “For example, the assumption that older people wouldn’t acclimate to video conferencing and that they wouldn’t be able to handle the technology, or that people who spoke a language than English can’t be served. I think we have to explore those assumptions and put extra effort into the navigators and the community health workers and whatever we have in society that we can leverage to get our patients comfortable on a digital platform so that we can deliver the care that they need through these crises.”
Brooke LeVasseur commented on the several ways that digital health can address some of the inequity issues: “This crisis has certainly pointed out the stark inequities that exist. I think as we look towards adapting and launching new ways of delivering care, we must look to eliminate those inequities that have existed for too long and take a thoughtful approach to questions such as how can telehealth really benefit all of society? Can we use telehealth to enable expanded networks? To connect patients to providers that not only understand my mental and my physical needs but also my cultural needs? I think there’s a lot of potential for us here to make a really positive change if we approach this new chapter with mindfulness of issues like this.”