WMIF MAIN SITE
2025 Event Site
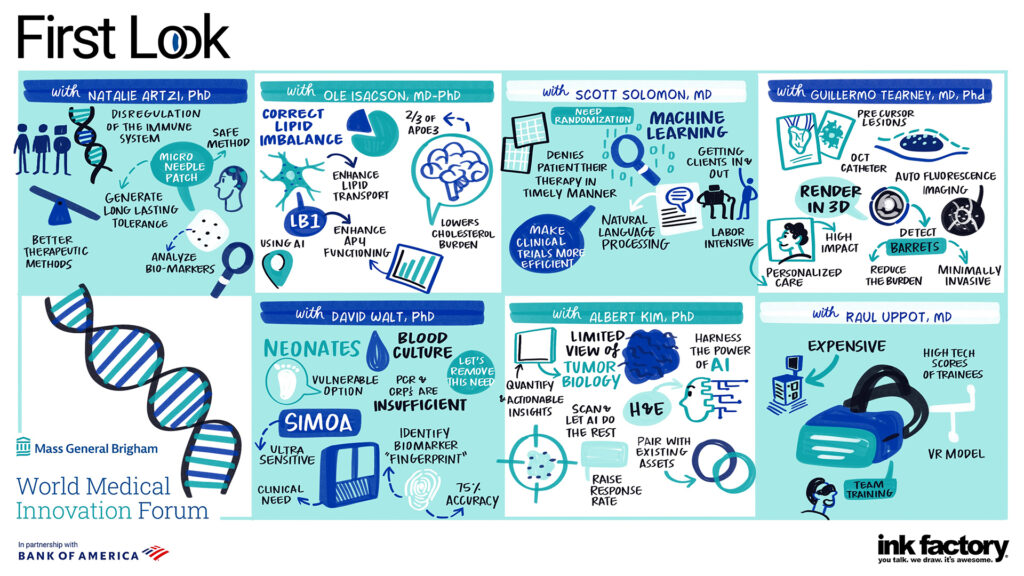
Covering a range of treatments, technologies, devices, and diagnostics, the presentations included therapies and solutions in oncology, inflammation and inflammatory diseases, neuroscience, AI and other specialties.
Technologies presented include:
• A drug patch to treat autoimmune skin disease
• A robotic bronchoscope that locates and treats hard-to-reach lung cancer
• First-in-class drug treatments for multiple myeloma
• An implantable brain-computer interface to help neurological disruptions
• The use of virtual reality to improve mental health resilience training
• New treatments for brain lipid abnormalities
• An app that integrates rheumatology patients’ outcomes into routine care
• How AI can streamline cardiovascular clinical trials
• Multimodal imaging for early disease detection
• A medical education platform integrating immersive virtual and real experiences
• Using saliva to diagnose sepsis in newborns
• How computational pathology can help precision oncology
• Using AI to manage blood pressure during Cesarean delivery
• A new cell therapy for regenerative medicine
Watch all of the First Look sessions.

Albert Bourla PhD, Chairman and CEO of Pfizer, spoke about his company’s dedication to science and how what is known about the immune system has advanced significantly since the COVID pandemic. Pfizer brought an mRNA vaccine to hundreds of millions around the world and validated the use of these vaccine therapies, said Paul Anderson MD, PhD, MGB’s Chief Academic Officer who introduced Bourla. The company also developed Paxlovid, considered the go-to medication for reducing COVID severity.
“Science is in the hard core of Pfizer’s DNA,” Bourla said. “We have demonstrated how effective we are. Our capabilities are impressive and will contribute to public health.”
The company is also setting the pace for other disease treatments, with more than 100 drugs in the pipeline to treat cancer and neurological disorders, among other diagnoses. “We know way more things now than we did three years back,” he said.
He also talked about AI, citing how technology and biology are “colliding together to create synergistic effects in unimaginable ways.” A company like Pfizer has collected a lot of research data over the past 30 years and compiling it in easy-to-access ways that AI can analyze is valuable.
“We publish the successes, but people don’t see all the data driving the failures,” he said. “We learn more from our failures and those are a significant asset when trying to develop medicines,” he said.
Watch Fireside chat with Albert Bourla PhD
Oncology’s New Paradigm:
How can clinicians best treat cancer? How is the current U.S. healthcare landscape contributing to how patients are diagnosed with and treated for cancer? How is it helpful to potentially diagnose cancers years before they would historically be detected?
These questions were asked and answered by an expert panel moderated by Keith Flaherty MD, Director of Clinical Research, Mass General Cancer Center, Professor of Medicine, Harvard Medical School; and Jason Zemansky PhD, SMid-Cap Biotech Analyst, BofA Global Research.
Shannon Stott PhD, Associate Investigator of the Krantz Family Center for Cancer Research d’Arbeloff Research School at Massachusetts General Hospital, touched upon studying tumor components that release messages from the immune system. “A combination that we are doing is expanding beyond looking at blood, but also looking at saliva and urine, specific to the cancer we are hoping to monitor,” she said.
Even with the innovations in diagnosing and treating cancer, there is still the problem of distribution and affordability, speakers noted. “Even with insurance, CAR-T is still expensive,” said Gregory Simon President, Simonovation.
In the past, when patients were diagnosed with pancreatic cancer, there were physicians who questioned what to do with the information since treatment options were limited. With new and emerging treatment innovations, he noted, “we can give people hope that they can do something about it,” he said.
Future of Cancer Care:
Treating cancer has evolved from what used to be surgery, chemotherapy and/or radiation to the oncologist becoming “part of a beautiful tapestry of care,” said Daphne Haas-Kogan MD, Chief, Enterprise Radiation Oncology, Mass General Brigham; Professor, Harvard Medical School.
That tapestry can include “things we use already and others that are aspirational goals. For 100 years, we would treat a man with prostate cancer with radiation. That man will get the same amount for weeks. But there might be a gas bubble passing through or he needs to urinate, and he has anatomy changes. AI has allowed us to make on the fly changes, scan and see what the anatomy looks like,” she said.
“With such differences, we can change the plan in a matter of seconds to deliver a more appropriate plan that day. That was never possible without AI and that’s possible now,” she said.
Benjamin Kann MD, Assistant Professor, Brigham and Women’s Hospital and Harvard Medical School, agreed. “I think there’s little doubt that AI will touch on every part of the cancer journey. AI will make impractical things practical… to make impossible things, possible.”
Watch Oncology’s New Paradigm: Technology
Watch Future of Delivering Cancer Care
Maura Healey, Governor of the Commonwealth of Massachusetts welcomed WMIF attendees to Massachusetts, home of healthcare’s innovation hub, explaining how the “culture of innovation is part of our DNA…it reflects our values of caring, collaboration, and leading in work that matters so much.”
Healey cited a number of “firsts” in the state including landing the Investor Catalyst Hub, the significant levels of venture capital and NIH funding, and growth in the life sciences sector. She also noted various biopharmaceutical and life sciences companies that are based in the state, including Eli Lilly opening in Fort Point Channel, Novo Nordisk launching space in Lexington, Moderna’s Cambridge location, Vertex re-signing a lease in the Seaport for 20 years, and Takeda extending its lease in Kendall Square until 2040.
The Governor also shared that the Healey-Driscoll Administration and the Massachusetts Life Sciences Center (MLSC) are announcing $19.8 million in life sciences funding aimed at advancing research and development, leveraging data science, addressing challenges in therapeutic delivery, and supporting initiatives focused on women’s health.
“There’s a reason why greater Boston is number one in innovation and punching way above its weight,” she concluded. “Whatever role you play, whether you work in a startup or a lab or in an established company, Massachusetts is your biggest partner. Thank you for all you do.”
Watch the 2024 WMIF Opening Remarks


Christophe Weber, President & CEO of Takeda, discussing the future of biopharma innovation, clinical trials, and industry-academia partnerships alongside fireside chat moderators, Jason Gerberry, Specialty Pharma and SMid-Cap Biotech Analyst, BofA Global Research and Allan Goldstein MD, Chief of Pediatric Surgery, Massachusetts General Hospital; Surgeon-in-Chief, Mass General for Children; Marshall K. Bartlett Professor of Surgery, Harvard Medical School

With more than 50 percent of hospital systems operating in the red since COVID and the subsequent financial crisis, what can be done to turn things around, asked moderator Andrew Bressler, Washington Healthcare Policy Analyst from Bank of America Global Research.
Academic healthcare systems are being threatened in a way they never have been before, said Anne Klibanski MD, President and CEO, Mass General Brigham. She noted that the delivery of AMC-based care hasn’t changed in 100 years. But investing in research, education, training the next generation of physicians and investing in community health can help solve its current challenges. Collaborating with the government or industry is another solution. “Industry partnerships are valuable,” she said. “You’ve got to get outside healthcare and look more broadly—that is critical. Think beyond your own healthcare system and think of things in different ways.
Panelists Rod Hochman, President & CEO, Providence, and Kevin Mahoney, CEO, University of Pennsylvania Health System, shared similar sentiments, including the role of value-based care and improving quality of care.
Klibanski said that creating Mass General Brigham Cancer, where patients can get all care at a flagship system through MGB’s specialty, outpatient and community hospitals, will also help lower costs. “Being able to democratize that care will benefit patients and lower the cost of that care,” she said.
Watch Delivering Care: New Tools, Evolving Challenges, Bold Aspirations